Platelet-rich plasma (PRP) and hyaluronic acid (HA)
Recent research suggests that combining platelet-rich plasma (PRP) with hyaluronic acid (HA) injections may be more effective than PRP or HA alone for knee osteoarthritis (1-5).
We are offering this combination of therapies to patients with knee osteoarthritis.
About PRP
PRP procedures use patients’ own blood to stimulate the healing of acute or chronic injuries. Blood contains immune cells and growth factors that are vital to injury repair.
PRP procedures supply injured tissue with a high concentration of immune cells, proteins, and growth factors that bolsters the tissue’s ability to rebuild and recover.
The concentrated immune cells, proteins, and growth factors are referred to as PRP or platelet-rich plasma.
About Hyaluronic Acid
Hyaluronic acid (HA) is a joint lubricant that is often injected into the knee to treat arthritis.
Hyaluronic acid is typically found in healthy joints as a component of synovial fluid. It acts as a shock absorber and allows for smooth movement of articular surfaces.
Patients with osteoarthritis often lack hyaluronic acid, which worsens joint function. Resupplying the knees with hyaluronic acid may improve the patient’s condition.
PRP + HA for Knee Osteoarthritis
Recent research has asserted that combining PRP and HA may be more effective than PRP or HA alone in knee osteoarthritis patients (1-5).
Knee osteoarthritis patients who receive both PRP and HA tend to have lower inflammatory cytokine levels, more pain relief, fewer cartilage breakdown markers, and better clinical outcomes than those who received PRP or HA alone (1-5).
How is PRP Made and Applied?
Patients should expect to be with us for about two hours. The procedure itself takes about 10-30 minutes.
Upon arrival, we check in with the patient and draw their blood.
In our lab, we separate the patient’s plasma from their red blood cells.
Next, we concentrate immune cells, proteins, and growth factors (the PRP) found within the plasma and prepare it for injection. This process takes about an hour.
Once the PRP is ready, we will begin the procedure. Using an ultrasound machine or fluoroscopy for visual guidance, Dr. Glowney injects numbing medication and then PRP into the patient’s injury.
The injected PRP stimulates injury repair over time.
For more information about the PRP procedure, see our PRP FAQ website page.
Making PRP Better Than The Rest
Creating effective PRP requires:
Customizing platelet concentration based on the patient’s particular needs
Adequately isolating platelets
Maintaining cell viability
Minimizing red blood cells’ presence in the PRP (for most orthopedic applications)
Customization
Currently, most clinics rely on premade PRP kits sold to them by medical device companies. These kits do not typically allow for customized PRP concentration, causing the clinic using them to take a one-size-fits-all approach to their patient’s treatments.
Customization of platelet concentration is critical to effective PRP treatment since each patient’s issue calls for a different potency of PRP. That’s because:
Patients’ platelet counts vary by age, gender, genetic factors, and lifestyle
Different parts of the body respond best to different concentrations of PRP
For example, nerves tend to recover best from low concentrations of PRP, but ligaments tend to do better with higher concentrations
Boulder Biologics’s PRP manufacturing strategy allows for customization of PRP concentration based on the patient’s platelet count, age, injury location, and injury severity, unlike clinics that use PRP kits. We also use a hemotologic analyzer to test every patient’s platelet count before preparing their PRP.
Our customization of PRP gives patients the best shot at recovery that PRP has the potential to provide.
Platelet Isolation and Viability
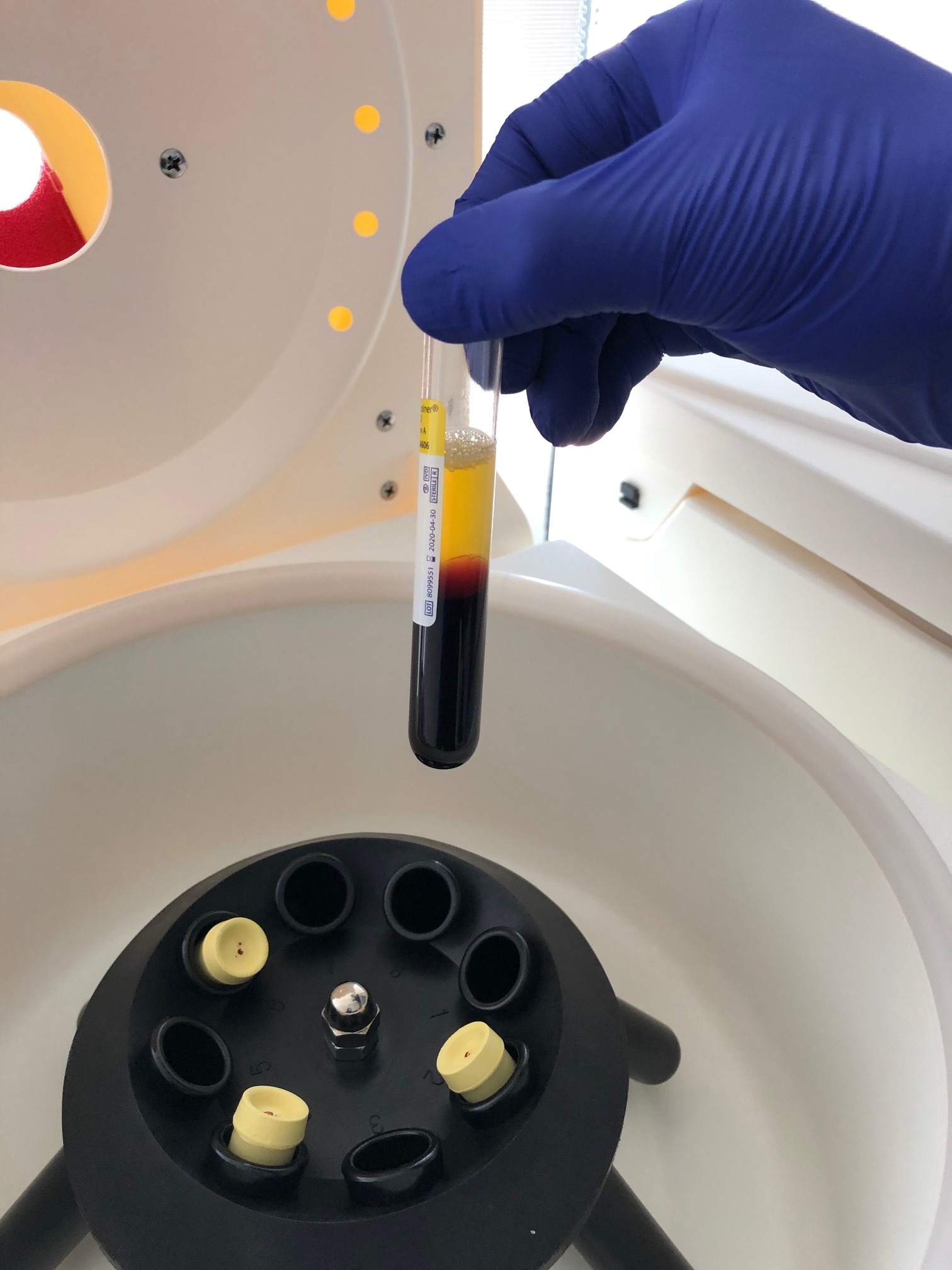
Centrifuges are machines that PRP clinics use to concentrate platelets from patients’ blood. The length of time patients’ blood spends in the centrifuge and the centrifuge’s speed influence the quality of the PRP. We set our centrifuges’ speed and duration for optimal cell viability and platelet isolation.
Red Blood Cells and Leukocytes
For most orthopedic applications, PRP should be low in leukocytes and red blood cells. At Boulder Biologics, our PRP manufacturing method allows for low red blood cell and leukocyte counts if it is called for.
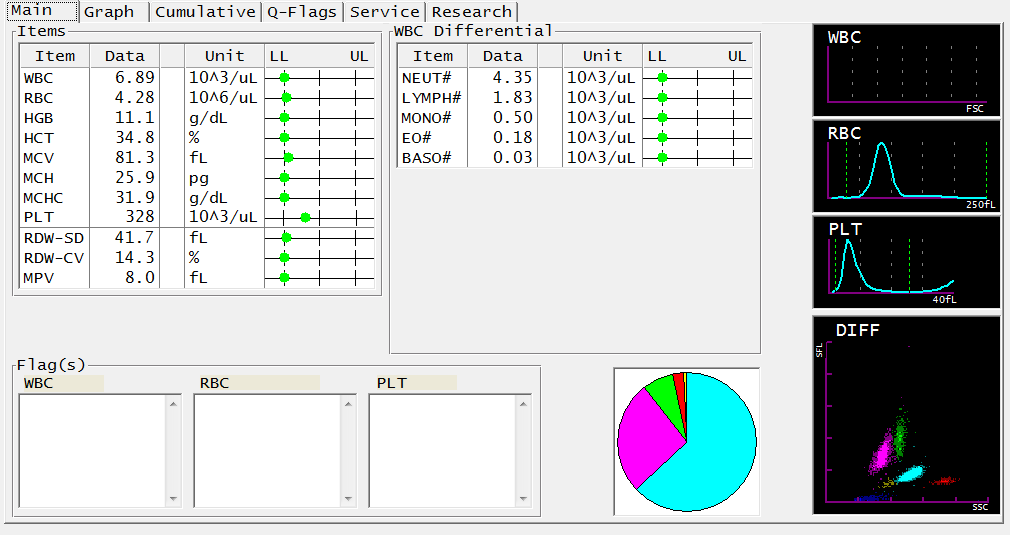
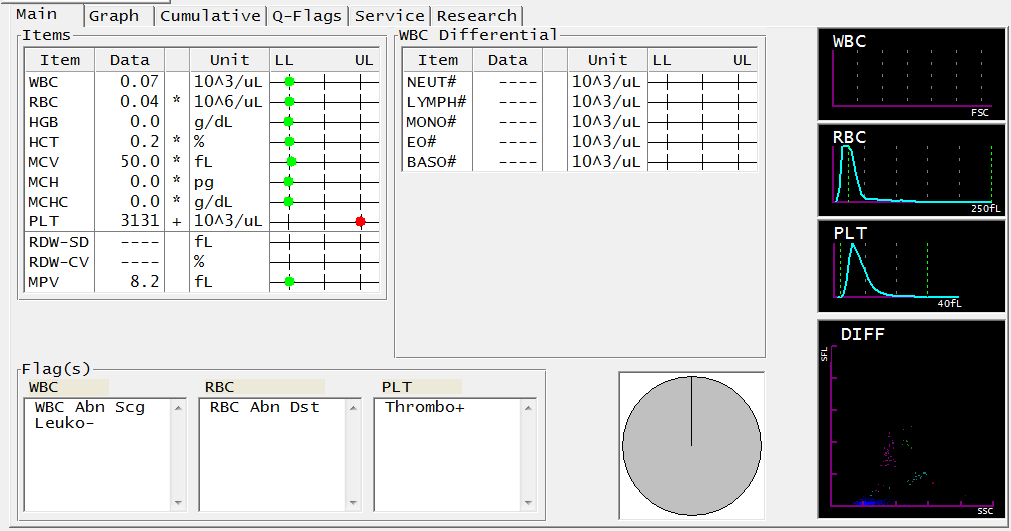
An example of PRP for an osteoarthritis patient is shown below. The first image is the patient’s CBC. The second image is an analysis of the PRP made for the patient.
Notice that platelets (PLT) are highly concentrated and the red blood cell (RBC) and leukocyte counts are very low in the second photo.
In the first image, the patient’s platelets are at 328, and in the second, they are at 3131.
In the first image, the patient’s RBCs are at 4.28, and in the second, they are at 0.04.
If you are interested in receiving PRP, we encourage you to reach out to us.
PRP: The Patient’s Initial CBC
PRP: The Resulting PRP Analysis
We have effectively eliminated 99% of the WBCs and RBCs in the PRP sample. We also obtained a near 10-fold concentration in platelets.
The platelet-plasma volume is separated from the other cells in the patient’s whole blood.
The platelets are concentrated from the patient’s plasma as pellets in the bottom of the conical tubes.
References
Lana JF, Weglein A, Sampson SE, Vicente EF, Huber SC, Souza CV, Ambach MA, Vincent H, Urban-Paffaro A, Onodera CM, Annichino-Bizzacchi JM, Santana MH, Belangero WD. Randomized controlled trial comparing hyaluronic acid, platelet-rich plasma and the combination of both in the treatment of mild and moderate osteoarthritis of the knee. J Stem Cells Regen Med. 2016 Nov 29;12(2):69-78. doi: 10.46582/jsrm.1202011. PMID: 28096631; PMCID: PMC5227106. https://pubmed.ncbi.nlm.nih.gov/28096631/
Yu W, Xu P, Huang G, Liu L. Clinical therapy of hyaluronic acid combined with platelet-rich plasma for the treatment of knee osteoarthritis. Exp Ther Med. 2018 Sep;16(3):2119-2125. doi: 10.3892/etm.2018.6412. Epub 2018 Jul 6. PMID: 30186448; PMCID: PMC6122407. https://pubmed.ncbi.nlm.nih.gov/30186448/
Papalia R, Zampogna B, Russo F, Torre G, De Salvatore S, Nobile C, Tirindelli MC, Grasso A, Vadalà G, Denaro V. The combined use of platelet rich plasma and hyaluronic acid: prospective results for the treatment of knee osteoarthritis. J Biol Regul Homeost Agents. 2019 Mar-Apr;33(2 Suppl. 1):21-28. XIX Congresso Nazionale S.I.C.O.O.P. Societa’ Italiana Chirurghi Ortopedici Dell’ospedalita’ Privata Accreditata. PMID: 31168999. https://pubmed.ncbi.nlm.nih.gov/31168999/
Xu Z, He Z, Shu L, Li X, Ma M, Ye C. Intra-Articular Platelet-Rich Plasma Combined With Hyaluronic Acid Injection for Knee Osteoarthritis Is Superior to Platelet-Rich Plasma or Hyaluronic Acid Alone in Inhibiting Inflammation and Improving Pain and Function. Arthroscopy. 2021 Mar;37(3):903-915. doi: 10.1016/j.arthro.2020.10.013. Epub 2020 Oct 20. PMID: 33091549. https://pubmed.ncbi.nlm.nih.gov/33091549/
Sun SF, Lin GC, Hsu CW, Lin HS, Liou IS, Wu SY. Comparing efficacy of intraarticular single crosslinked Hyaluronan (HYAJOINT Plus) and platelet-rich plasma (PRP) versus PRP alone for treating knee osteoarthritis. Sci Rep. 2021 Jan 8;11(1):140. doi: 10.1038/s41598-020-80333-x. PMID: 33420185; PMCID: PMC7794411 https://pubmed.ncbi.nlm.nih.gov/33420185/